Women’s Health

PHYSIO DOWN UNDER SERVICES
Pelvic floor physiotherapy is similar to other types of physiotherapy. Firstly, your therapist will begin by learning about you. You will discuss your past medical history, your current lifestyle, symptoms, and your goals. Secondly, your physiotherapist will watch you move and test your strength and mobility. Your therapist may recommend an internal exam to test your pelvic floor muscles, but it is never mandatory. Thirdly, your physio will discuss their findings and collaborate with you on a plan of care. Treatment plans usually consist of exercises, education, and building helpful habits. They will go through exercises with you and may send you an email with exercise videos so you can continue your therapy at home. In conclusion, we want you to leave your physiotherapy session feeling comfortable, confident, and educated about your condition.

Urinary Incontinence
Urinary incontinence is any involuntary loss of urine. Leaking of urine is common but definitely not normal. Stress urinary incontinence (SUI), is the involuntary leakage of urine with activities that increase pressure inside the abdomen, such as coughing, sneezing, laughing, jumping, running. Whereas, urge urinary incontinence (UUI), is the involuntary loss of urine associated with a sudden and strong urge to urinate. SUI is more common in women than UUI, but you can get a combination of the 2 which is called mixed urinary incontinence.
For both conditions there is good evidence that they can be successfully managed with conservative measures.
A treatment program for urinary incontinence at Physio Down Under can include:
- Optimising breathing patterns
- Assessing and retraining abdominal muscle recruitment
- Pelvic floor rehabilitation
- Postural changes
- Lifting and movement education
- Bowel optimisation
- Bladder retraining and calming techniques
- Electrical stimulation (vaginal and/or external)
- Fitting a continence support device
- Referral for a surgical consult in some more severe non responding cases may be necessary
Pelvic Organ Prolapse
Pelvic organ prolapse occurs when one or more of your pelvic organs (bladder, uterus, rectum), loses internal connective tissue support, resulting in a drop of the affected organ onto the vaginal wall. Approximately 50% of women will have a prolapse, but not all will be symptomatic or aware of it.
Symptoms vary, but often include:
- A feeling of heaviness/pressure by the vagina
- Noticing a lump or bulge at the vagina
- Difficulty wearing a tampon or menstrual cup
- Difficulty with fully emptying your bladder or bowel
Physiotherapy can be highly effective in reducing the symptoms and stag of POP, especially in mild to moderate cases.
A treatment program for prolapse at Physio Down Under can include:
- Optimising breathing patterns
- Assessing and retraining abdominal muscle recruitment
- Pelvic floor rehabilitation
- Postural changes
- Lifting and movement education
- Bowel optimisation
- Vaginal support pessary
- Referral for a surgical consult in some more severe non responding cases may be necessary


Post-Natal Check
Having a women’s health physio postnatal check at around 6-8 weeks post birth, can help pick up any issues early, and will help guide you back to exercise safely.
It may involve:
- Posture assessment (including for breast/bottle feeding)
- Assessing and managing any abdominal muscle separation
- Assessing and managing any pelvic floor muscle dysfunction
- Individualised advice on safe return to exercise
- Addressing any concerns regarding painful sexual intercourse
You are welcome to come in earlier than 6 weeks postnatal if you have any specific concerns such as back pain, issues with bladder or bowel control or pelvic heaviness.
Pelvic Floor Muscle Dysfunction
This can include a weak pelvic floor, but also an overactive, tight pelvic floor. Both of which are managed differently and need careful assessment. Research has shown that up to 40% of women perform an incorrect pelvic floor muscle contraction, which can result in more harm than good. A correct pelvic floor muscle contraction, results in a distinct ‘squeeze and lift’ around the vagina followed by an effective relaxation of the muscles.
Rehabilitation of the pelvic floor can include:
- Pelvic floor strengthening
- Pelvic floor downtraining
- Optimising pelvic floor co-ordination and motor control
- EMG
- Real time ultrasound
- Electrical stimulation


Birth Preparation
We now have excellent evidence that a prenatal pelvic floor physiotherapy appointment can help with labour preparation and delivery. We would ideally like to see you in your 2nd trimester but if possible, by 34 weeks at the latest. We can see you earlier than your 2nd trimester if you are having any specific concerns with back, pelvic or joint pain or any bladder or bowels issues.
The initial appointment is 60 minutes and will consist of a detailed history taking followed by an explanation regarding the assessment procedure.
- Depending upon your symptoms, your physical examination may consist of an internal pelvic floor examination. This will only be conducted with your full informed consent and can only be done in pregnancy if you do not have a high risk pregnancy.
- Your management plan will prioritise your goals, in combination with your signs and symptoms.
The First appointment would be a 60 minute session that would include (but not necessarily limited to):
- a posture check
- assess your breathing
- pelvic floor assessment including teaching correct pelvic floor muscle technique
- Assess correct pushing and relaxation of your pelvic floor in preparation for delivery (real time ultrasound may be used for this)
- Starting you on an appropriate pelvic floor muscle training program
- Going through pelvic floor friendly delivery techniques
- Teaching perineal massage (the Epino can also be discussed)
- Going postnatal care advice
Follow up appointments are routinely 45 minutes unless your physiotherapist advises you otherwise.
Preparing your pelvic floor for pregnancy and birth is not just about strengthening it. The strength, endurance and functional coordination are very useful during pregnancy but when it’s time to labour and give birth we need your muscles to soften and lengthen to allow your baby to descend and birth.
Many women struggle to effectively release and lengthen their pelvic floor muscles and using real time ultrasound is an excellent tool to facilitate a correct pushing technique.
Research demonstrates that having a pelvic floor that is able to lengthen on pushing, leads to a significantly lower incidence of severe perineal tears, and a significantly shorter second stage of labour (the pushing time).
At any point during the pregnancy, we go through the risks and benefits, to you as the mother, associated with normal vaginal delivery, instrumental deliveries, caesarean sections, labour positions, epidurals, perineal tears and episiotomies. This information is discussed to empower you to make informed decisions during your labour and delivery, or at a bare minimum to know what is happening if an emergency situation occurs.
Your Obstetrician does their utmost to assist you in having the delivery of your choice. Unfortunately, things don’t always go to plan, interventions are needed, and that’s okay. What is important is that both you and your baby are healthy. Understanding what is happening, and why, if things don’t go to plan is very powerful for both you and your partner. Being able to make informed decisions when the opportunity arises is also invaluable in helping you deal with the change of plan.
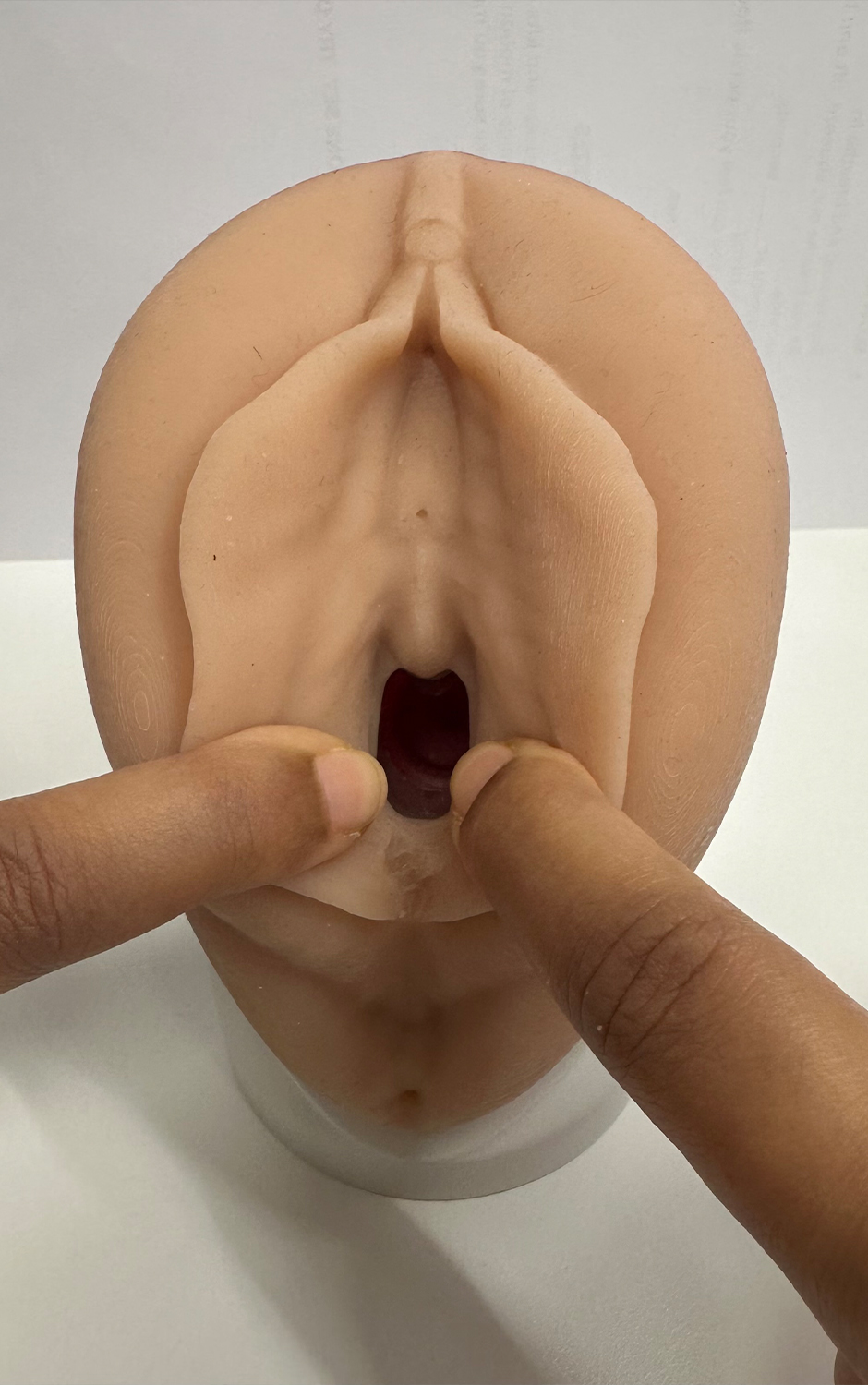
Perineal Massage
Perineal massage is a technique used to stretch the perineum (the area between the vagina and anus) in preparation for childbirth. The goal is to increase the elasticity of the perineal tissue, resulting in significantly reduced risk of severe perineal tears and a reduced risk of post-natal symptoms.. It can also be a way to become more familiar with the area and manage any discomfort that may arise during labour by practicing your breathing techniques.
Around the 34th week of pregnancy, we teach you perineal massage. You may choose to do this yourself, you may prefer your partner to do it, or you may prefer one of our Pelvic Health Physiotherapists to do the release for you. Your partner is welcome to attend this session so we can teach them how to the massage.
Perineal massage has been shown to:
- reduce the risk of episiotomy
- reduce the risk of grade 3 & 4 perineal tears
- decrease the severity of postpartum perineal pain
- reduce the risk of anal incontinence
- reduce the second stage of labour

Bowel Disorders
A healthy bowel should allow you to hold on for a short time after you first feel the urge to do a poo, do a poo within about a minute of sitting down on the toilet, easily and without pain (not having to push too hard) and feeling empty afterwards. A dysfunctional bowel has been shown to contribute to general pelvic floor muscle dysfunction disorders such as urinary urgency, urinary incontinence and pelvic organ prolapse. An optimal pelvic floor health can promote healthy bowel function.
At Physio Down Under common bowel conditions that we treat include:
- Constipation
- Urgency (being afraid you won’t make it to the toilet on time)
- Leakage of faeces
- Difficulty controlling wind
- Difficulty emptying your bowel
Physiotherapy for bowel dysfunction can be highly effective and make a huge difference to a woman’s quality of life and management can include:
- Lifestyle and diet advice
- Education and strategies for correct defecation dynamics
- Pelvic floor muscle down training and teaching relaxation strategies for optimal evacuation
- Pelvic floor release
- Education and building awareness of pelvic floor muscle strengthening
We will usually refer and work with other health practitioners such as colorectal surgeon, dietician, functional medicine practitioner, nutritionist, naturopath, when indicated.
Abdominal Muscle Separation
Diastasis Rectus Abdominis (DRA), commonly known as abdominal separation, is the widening and thinning of the most superficial layer of the abdominal muscles (rectus abdominis or the 6-pack muscles), and occurs when the connective tissue (the linea alba) which joins the two sides of the muscles stretches and widens. It is a condition that occurs to varying degrees in all pregnant women during the later stages of the third trimester as the abdominal wall stretches to accommodate the growing baby. This natural widening normally resolves itself in the first few weeks after delivery, however, approximately 30% of women continue to have a bothersome diastasis beyond three months postpartum.
The reasons for this remain largely unknown, and it is widely accepted that there is a need for continued research. However, current hypothesis indicate that collagen type and genetic predisposition may play a strong role. In the past, there were lists of contraindicated exercises and activities, but we now know this is no longer helpful and each woman with a diastasis has different abilities and strength and will benefit from a more individualised approach.
Not all women with diastasis present with bothersome or limiting issues; however, some find that it can impact their ability to do simple daily tasks such as sitting themselves up from lying, twisting to lift up a load, and even effectively emptying their bowels without excessive straining. Many women with a significant DRA also report feeling upset with the appearance of their distended abdominal wall, as they often get asked if they are still pregnant and this has been shown to negatively affect a woman’s self-esteem
At Physio Down Under, we use a whole-body approach in the assessment and treatment of DRA, which includes addressing the following:
- Posture
- Breathing
- Real time imaging ultrasound and manual palpation to measure not only the ‘gap’ between the muscles, but also the quality of the tissues of that ‘gap’ (ie. the depth and thickness of the linea alba)
- Pelvic floor function
- Pain/ Discomfort
- Functional strength and ability to manage core pressure
- Identify and correct compensations and imbalances
- Identify specific exercises that can help reduce the ‘gap’, strengthen the connective tissue and all supporting muscles
Ultimately, at Physio Down Under, we strive to support and empower women to become strong and return safely to their activities of choice.


Pregnancy Musculoskeletal
Musculoskeletal conditions in pregnancy are relatively common due to the significant physical changes that occur in a woman's body during this time. Some of the common musculoskeletal issues experienced during pregnancy include:
- Low back pain: This is one of the most prevalent musculoskeletal complaints during pregnancy, affecting about two-thirds of pregnant women. The added weight of the baby, changes in posture, and hormonal changes can contribute to strain on the lower back.
- Pelvic girdle pain (PGP): Formerly known as symphysis pubis dysfunction (SPD), PGP involves pain in the pelvic joints and can range from mild discomfort to severe pain. Risk factors for developing PGP in pregnancy is still inconclusive but is thought include a past history of back pain, PGP in a previous pregnancy, low satisfaction at work and high levels of stress.
- Round ligament pain: As the uterus expands during pregnancy, the round ligaments that support it can stretch and cause sharp, shooting pains in the lower abdomen or groin area, often felt with sudden movements,
- Carpal tunnel syndrome: Some women experience symptoms of numbness, tingling, and weakness in the hands and wrists, due to swelling and pressure on the nerves.
- Leg cramps: These are common in pregnancy, especially during the second and third trimesters, and are thought to be due to changes in circulation and increased pressure on leg muscles.
- Sciatica: Pressure on the sciatic nerve, often due to the growing uterus, can cause pain, numbness, or tingling that radiates from the lower back down the leg.
At Physio Down Under, we manage musculoskeletal conditions during pregnancy using a variety of strategies, including:
- Exercise: Gentle exercises such as prenatal yoga, swimming, or walking can help strengthen muscles, improve posture, and alleviate discomfort.
- Supportive devices: Proprioceptive taping, supportive pelvic girdle and abdominal belts and education on using pillows can help relieve pressure on the back and pelvis.
- Posture and movement adjustments: Being mindful of posture, especially when sitting or standing for long periods, modifying how to change positions and getting in and out of bed, dressing the lower half of the body, getting in and out of a car can all help reduce strain on the back and pelvis.
- Manual therapy: Manual techniques to help manage pain and improve mobility and function.
It's essential for pregnant women experiencing musculoskeletal issues to communicate with their healthcare providers to ensure the most appropriate and safe management plan for their individual needs.
Gynaecological Surgery
Pelvic health physiotherapists play an important role in assessing patients pre and post operatively prior to a number of gynaecological surgeries including continence procedures, prolapse surgery and hysterectomy.
It would be ideal to assess you pre-operatively as we usually like to address bladder and bowel habits and train a correct pelvic floor activation prior to having surgery. This will allow optimal time to set up good habits and will mean they won’t be overwhelmed with information after surgery.
Your recovery immediately postoperatively and in the weeks following surgery can be made more comfortable and less daunting with some simple strategies taught to you by a Physiotherapist. We know that your long-term outcomes from these surgeries can be affected by many factors such as:
- Straining to empty your bladder or bowel
- Returning to strenuous activities, heavy lifting, and high impact exercise too soon in your recovery
- Poor pelvic floor and abdominal muscle function
Sometimes women experience bladder leakage or painful sex following their operation, and Physiotherapy treatment can help with these problems too.


Pelvic Pain
This often involves pain during sexual intercourse (dyspareunia), but can involve abdominal pain below the belly button, that affects a woman’s day-to-day life.
Depending on symptoms and assessment findings, treatment can involve:
- Pelvic floor downtraining
- Breathing pattern education
- Pain cycle education
Endometriosis
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, often causing cyclical pain, such as during ovulation and/ or days before the period starts. Other common associated symptoms include low back and pelvic pain, bladder, bowel concerns and deep pain with sexual intercourse.
Pelvic health physiotherapy plays a valuable role in managing endometriosis. At Physio Down Under, we focus on addressing musculoskeletal dysfunctions, including those related to the pelvic floor muscles, to alleviate symptoms and improve quality of life for individuals with endometriosis. Here's how pelvic health physiotherapy can help:
- Pain Management: Assist in reducing pelvic pain associated with endometriosis through various techniques. This may include manual therapy, such as internal and/ or external massage or myofascial release, to release tension in the pelvic floor, abdominal muscles and surrounding tissues. Additionally, exercises and stretches tailored to the individual's needs can help improve flexibility, reduce muscle spasms, and alleviate pain.
- Pelvic Floor Dysfunction: Endometriosis can contribute to pelvic floor dysfunction, including overactive (too tense) pelvic floor muscles. Pelvic physiotherapists assess and address these dysfunctions through techniques such as biofeedback, pelvic floor muscle relaxation exercises, and techniques to restore proper function and coordination of the pelvic floor muscles.
- Improving Bowel and Bladder Function: Endometriosis can impact bowel and bladder function, leading to symptoms such as urinary urgency, frequency, constipation, or painful bowel movements. Pelvic physiotherapy interventions may include education on bladder and bowel habits, pelvic floor muscle training to improve control and coordination, and manual therapy techniques to address any associated dysfunctions.
- Pre and Post-surgical Rehabilitation: For individuals undergoing surgery for endometriosis, pelvic physiotherapy can play a crucial role in optimising pelvic floor function both before and after surgery. Pre-surgical physiotherapy may focus on down training and reducing tension in the pelvic floor muscles, while post-surgical rehabilitation can aid in recovery, reduce scar tissue formation, and improve mobility and function.
- Education and Self-management: Education on pain management strategies, ergonomic modifications, and lifestyle changes to help individuals with endometriosis better manage their symptoms on a day-to-day basis. This empowers patients to take an active role in their treatment and improves their overall well-being.
It's important for individuals with endometriosis to work with a multidisciplinary healthcare team, including gynaecologists, pain specialists, psychologists, and pelvic health physiotherapists. The ultimate aim is to develop a comprehensive treatment plan tailored to their specific needs and provide holistic care that addresses both the physical and emotional aspects of this complex condition.


Vaginismus
Vaginismus (also termed Genito-pelvic pain penetration disorder) is a condition characterised by involuntary spasms or contractions of the muscles around the vagina, particularly the pelvic floor muscles. These contractions can make penetration painful, difficult, or even impossible. It's important to note that vaginismus is not a conscious choice or a result of lack of arousal; it's a reflex reaction that occurs involuntarily.
There are two main types of vaginismus:
- Primary: This occurs when a person has never been able to have penetrative intercourse due to the involuntary muscle contractions. It often becomes apparent during attempts to insert a tampon, intercourse or gynaecological exams.
- Secondary: This develops after a period of normal sexual function. It can occur due to various factors such as trauma (physical or emotional), painful scars after an episiotomy or perineal tear, pelvic surgery, medical conditions, or relationship issues.
Symptoms of vaginismus can vary in severity and may include:
- Difficulty or inability to insert tampons, fingers, or penis into the vagina
- Pain or discomfort during attempted penetration
- Tensing or tightening of pelvic floor muscles in anticipation of penetration
- Anxiety or fear related to sexual activity or gynaecological exams
The exact cause of vaginismus can be complex and multifaceted, involving physical, psychological, and relational factors. Some common contributing factors may include:
- Traumatic sexual experiences (physical or emotional)
- Fear of pain or discomfort during penetration
- Anxiety or stress related to sex, intimacy, or past sexual trauma
- Relationship issues, communication problems, or lack of trust
- Medical conditions such as infections, endometriosis, or pelvic floor disorders
- Cultural or religious beliefs that influence attitudes towards sex
Treatment for vaginismus typically involves a multidisciplinary approach that addresses both the physical and emotional aspects of the condition. This may include:
- Pelvic floor physiotherapy: Techniques such as relaxation exercises, biofeedback, and manual therapy can help to relax and desensitize the pelvic floor muscles.
- Education and self-help techniques: Learning about sexual anatomy, arousal, and relaxation techniques can help individuals understand their bodies and develop strategies to manage symptoms.
- Gradual desensitization: Gradually exposing oneself to the sensations of penetration, starting with small, non-threatening objects such as tapered vaginal dilators and progressing to larger sizes that resemble the anatomy of the penis. This type of therapy can help desensitize the pelvic floor and reduce anxiety.
- Counselling or therapy: Cognitive-behavioural therapy (CBT), psychotherapy, or sex therapy can help individuals address underlying psychological factors, overcome fears or anxieties, and improve communication and intimacy within relationships. We work closely with and refer our patients to therapists who have extensive experience working with this sensitive condition.
Overall, the prognosis for vaginismus is generally good with appropriate treatment and support. It's essential for individuals experiencing symptoms of vaginismus to seek help from healthcare professionals who specialise in sexual health and pelvic floor disorders. With the right approach, many individuals can overcome vaginismus and enjoy fulfilling sexual relationships.
Pelvic Venous Disorders
Pelvic physiotherapy, while not a primary treatment for pelvic venous disorders, can play a supportive role in managing symptoms and improving quality of life for individuals with these conditions. Pelvic venous disorders, such as pelvic congestion syndrome (PCS) or pelvic varicose veins, involve the abnormal enlargement or dysfunction of veins in the pelvic region, often leading to symptoms such as pelvic pain, heaviness, discomfort, pain after sexual intercourse and swelling.
Pelvic physiotherapy may contribute to the management of pelvic venous disorders in the following ways:
- Pain Management: Pelvic physiotherapy techniques, such as manual therapy, myofascial release, and gentle exercises (including the Pilates method), can help reduce pelvic pain associated with venous congestion. Therapists may target specific tension points in the pelvic floor muscles and surrounding tissues to alleviate discomfort.
- Improving Circulation: Certain exercises and movement patterns can help improve blood circulation in the pelvic region, and this may help alleviate symptoms of venous congestion. This includes exercises to promote pelvic floor muscle tone, lymphatic drainage and reduce fluid retention, as well as techniques to enhance venous return to the heart.
- Pelvic Floor Function: Pelvic venous disorders can impact pelvic floor muscle function, leading to symptoms such as pelvic floor dysfunction or bladder and bowel issues. Pelvic physiotherapy interventions may include pelvic floor muscle training, biofeedback, and relaxation techniques to optimize pelvic floor function and reduce symptoms of pain and tension.
- Posture and Alignment: Poor posture and pelvic alignment can contribute to venous congestion and exacerbate symptoms of pelvic venous disorders. Pelvic physiotherapists can assess and address biomechanical issues, provide ergonomic advice, and prescribe exercises to improve posture and pelvic alignment, thereby reducing pressure on pelvic veins.
- Education and Self-management: Education on lifestyle modifications, including activity modification, and strategies for symptom management can be valuable to empower individuals with pelvic venous disorders to take an active role in their treatment and improve their overall well-being.
Individuals with pelvic venous disorders should work closely with a multidisciplinary healthcare team, including vascular specialists, gynecologists, psychologists, and pelvic physiotherapists, to develop a personalized treatment plan tailored to their needs and goals. At Physio Down Under we work closely with highly competent specialist clinics, such as The Harley Street and Venus Clinic.


Mastitis/Blocked Milk Ducts
It has been estimated that two thirds of women will experience blocked milk ducts at some time during their breastfeeding journey. It is thought that excess milk in the breast causes inflamed and swollen breast tissue that can surround and close a duct. At times this inflammation of the breast may lead to mastitis. Anything that hinders milk good milk drainage could cause breast inflammation. Examples include poor positioning (the way baby is held to breastfeed) and latch, a tight bra or shoulder bag/back pack strap pressing on breast tissue, or even breastfeeding to a schedule instead of on demand. Previous breast surgery, scar tissue, a finger pressing into the breast, nipple piercing or a blocked nipple pore could also cause blocked ducts.
The most common symptoms are:
- A swollen, red and shiny, or tender breast
- Pain while breastfeeding
- Flu-like symptoms including fever & chills
- Firm mass or lumpy breast area that doesn't soften well after a breastfeed
The use of therapeutic ultrasound can be useful in the resolution of symptoms (pain and lump) associated with blocked milk ducts. The number of treatments needed varies from 1-5, usually on a daily basis. Our physiotherapists are also trained to do and teach lymphatic massage for blocked milk ducts and in the use of kineseotaping to help with lymphatic drainage of blocked milk ducts. Other strategies include using cold therapy, breast-feeding safe non-steroidal anti-inflammatories and rest can all help to reduce the inflammation of the breast.
Vaginal Support Pessaries
A pessary is a soft silicone device that is placed inside the vagina to provide support for pelvic organ descent. It is designed to support the vaginal wall and assist the connective tissue that would be normally be providing support to the pelvic organs.
There are many different types of pessaries, including ring, cube and gellhorn. The symptoms of prolapse can be reduced by using a pessary and can allow a woman to return to what would otherwise be aggravating or high-risk activities for her prolapse.
A self-managed pessary will be taken in and out by yourself, and regular reviews will be with your physiotherapist, in conjunction with your GP or gynaecologist. Pessaries can be life changing for some woman and are an excellent conservative option to try prior to considering surgery for prolapse.
Please be aware that the process of fitting a pessary involves 2 separate appointments, the initial trial where different pessaries are trialled to find the ideal style and size for you, and a final fitting usually 2 weeks later with your own pessary where you will learn to insert and remove the pessary independently. If you are thinking about getting a pessary fitted, please make an appointment with Tamara Gerdis.


Menopause
Menopause is a natural process which, like the onset of menstruation, is completely normal. Menopause is a phase of a woman’s life that marks the end to her ability to get pregnant and an end to her menstrual cycles. The average age for menopause is 51 but peri-menopause, when a women’s hormones start to change, can start 5-10 years before her periods cease.
Each woman’s experience of the menopause is different. As hormone production by the ovaries start to fall most women do experience some kind of symptoms, although the type and extent of these can vary widely. The falling levels of oestrogen can lead to a group of genital and urinary symptoms that are called genitourinary syndrome of the menopause or GSM. Some of the symptoms of GSM you may notice include;
- Itching, burning or discomfort in the vaginal area or when emptying your bladder
- Vaginal examinations or smear tests become uncomfortable. If you are still using tampons these can start to feel uncomfortable.
- More frequent infections of the urinary tract (UTI) and or vaginal infections
- Symptoms of pelvic organ prolapse
- Decreased libido
- Vaginal dryness
- Increased frequency and urgency to empty your bladder.
- Leakage of urine if you cough, sneeze, laugh or move suddenly known as stress urinary incontinence
- The changes in the tissues make them more fragile so penetration can cause small tears and you may also experience bleeding after intercourse
Other changes that may occur during menopause include:
- Decreased bone density and muscle mass
- Hair loss
- Facial hair growth
- Hot flushes
- Chills
- Weight gain/slowed metabolic rates
- Painful/stiff/achy joints
- Headaches
- Memory problems
- Anxiety or depression
At Physio Down Under, we like to explain Women’s Health Physiotherapy as care for women at every stage of their life. Although there is often a lot of focus on Women’s Health Physiotherapy for pregnancy and the child-bearing years (this is often what is most recognized by the public), we also specialise in treating bladder and bowel dysfunction, pelvic organ prolapse, pelvic/abdominal pain, post-surgery sexual dysfunction and are experts in exercise prescription. These issues may occur at any life-stage, but as you can see from the menopause symptoms list, they are commonly experienced in menopause.

Osteopenia / Osteoporosis
Osteopenia and osteoporosis are conditions characterised by decreased bone density, making bones weaker and more susceptible to fractures. Osteopenia is a precursor to osteoporosis and signifies lower bone density than normal but not low enough to be classified as osteoporosis. These conditions often develop silently over years and are more common in older adults, particularly women post-menopause.
Factors contributing to osteopenia and osteoporosis include:
- Aging, as bones naturally lose density over time
- Hormonal changes, especially decreased oestrogen in women after menopause
- Inadequate calcium and vitamin D intake
- Sedentary lifestyle or lack of weight-bearing exercise
- Smoking, excessive alcohol consumption, and certain medications
Early stages of osteopenia and osteoporosis may not cause noticeable symptoms until a fracture occurs. Common symptoms include:
- Loss of height over time
- Back pain due to fractures or collapsed vertebrae
- Increased risk of fractures, especially in the hip, spine, or wrist
Diagnosis involves bone density testing (DEXA scan) to measure bone mineral density and assess fracture risk. Our physiotherapy clinic plays a crucial role in managing osteopenia and osteoporosis through personalised treatment plans.
Our physiotherapists employ specialised techniques to improve bone health and reduce fracture risk:
- Exercise Programs: Weight-bearing exercises and resistance training to strengthen bones and muscles, improving balance and coordination.
- Fall Prevention Strategies: Balance training and gait exercises to reduce the risk of falls, a common cause of fractures.
- Posture Correction: Education on proper posture and body mechanics to prevent spinal fractures.
- Pain Management: Techniques such as manual therapy and modalities to alleviate pain associated with fractures or musculoskeletal issues.
We collaborate closely with your healthcare team, including primary care physicians and specialists, to ensure comprehensive care. Our goal is to enhance your bone health, functional mobility, and overall quality of life through evidence-based physiotherapy interventions.
Early action against osteopenia can significantly slow or prevent its progression to osteoporosis.
Real time ultrasound imaging and EMG
This type of technology adds to the assessment and treatment of women’s health conditions, like diastasis recti and pelvic floor dysfunction.
The image or graph of the deep abdominal and pelvic floor muscles contracting and relaxing give women instant visual feedback, which can translate into better muscular control.
The ultrasound image allows the physiotherapist and the patient to see in real time the effect their pelvic floor muscles have on pelvic organs, such as the bladder, during a cough or a strenuous movement. The probe is placed externally over the lower belly or on the perineum, and the scan is performed lying down and/or standing up.
EMG is a procedure that evaluates the condition of muscles and nerve cells that control them. These nerves cells are known as motor neurons, and they transmit electrical signals that cause muscles to contract or relax. An EMG transforms these signals into graphs or numbers, helping physiotherapists assess whether a woman’s pelvic floor muscles are weak, slow at contracting or unable to fully relax. An internal probe or external electrodes may be used to assess pelvic floor muscles with EMG.
At present, we cannot use ultrasound or EMG to diagnose specific conditions. This has to be done by a specialist doctor like a radiologist. However, appropriately trained physiotherapists can use this type of equipment to enhance their assessment and to provide their patients with valuable biofeedback during treatment.

Physio Down Under Pte Ltd
Address
491B River Valley Road
Valley Point (Office Tower)
Unit #04-01A
Singapore
248373
© Copyright 2024 | All Rights Reserved | Physio Down Under | Privacy Policy
